We’re changing the way the world fights poverty and disease
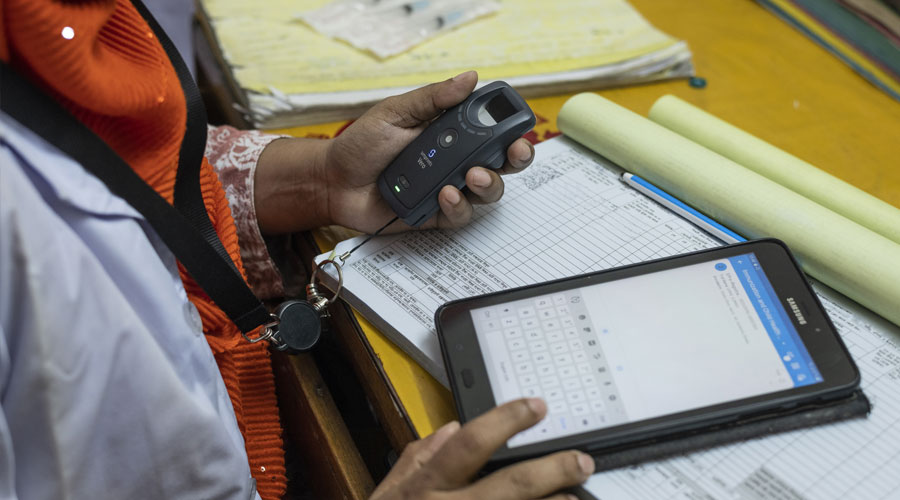
We build technology that radically increases transparency and effectiveness in global development, making sure that every vaccine, every dollar, every public good reaches the people who need them most.
Deploy Simprints

The identity challenge
- 850 million people globally lack formal identity.
- 1 in 4 children born today are not registered anywhere.
- Patient misidentification occurs in over 90% of medical facilities, contributing to almost 35% of all frontline health records containing inaccurate or false data.
- The most vulnerable populations, often the ones without any formal ID, are missing out on critical health and humanitarian support.
3,501,356
People enrolled
17
Countries reached
4,751
Active users
Impact across sectors
Lack of identification is a cross-cutting challenge. We build digital ID tools backed by inclusive AI algorithms to empower frontline teams to verify, monitor, and optimise the delivery of essential services.
Maternal health
Every mother and child is protected before, during, and after pregnancy
Immunisations
Every 'zero-dose' or partially immunised child is fully vaccinated
Clinical trials
Accurate and clean data is available to validate research hypotheses
Infectious diseases
Every patient receives treatment to protect them from HIV, Malaria, and more
Cash & humanitarian aid
Humanitarian aid reaches the right people at the right time
Monitoring & evaluation
Teams can make data-driven decisions with real-time and accurate M&E data
Simprints products
Our products are designed for impact.
You can implement our open-source biometric ID platform alongside powerful algorithms that suit your project. We’ll help you unlock data insights and power project dashboards.
Learn more
Project services
We design a solution that is tailored to you.
As your impact partner, we’ll integrate our cutting-edge biometric tools into your existing platforms, with bespoke configuration, a choice of modality, full training and ongoing support to ensure we build a foundation for sustainable success.
Find out more